Plantar Fasciitis During Pregnancy: Causes, Heel Pain Relief, and Safe Treatment Options
Plantar fasciitis in pregnancy can cause heel pain and discomfort. Learn safe relief options, symptoms to watch for, and care guidance from FAS The Woodlands.
Flaky, itchy feet are a common issue but figuring out what’s causing them isn’t always easy. You might assume it’s just dryness from weather or shoes, but in many cases, those symptoms could actually point to a fungal infection like athlete’s foot. So how do you know what you're really dealing with?
In this blog, we’ll compare foot fungus vs dry skin, highlighting how the two conditions differ, how they overlap, and when it’s time to bring in a podiatrist for answers (and relief). Understanding the root cause is the first step toward healthier, more comfortable feet.
Foot fungus, especially athlete’s foot (tinea pedis), is caused by fungal organisms that thrive in warm, moist environments like locker rooms, communal showers, tight shoes, and even your own socks. It spreads easily through skin-to-skin contact or contaminated surfaces, and it can linger for a long time if left untreated.
Foot fungus can be contagious, and the symptoms often worsen over time without proper treatment. Learn more about how foot fungus spreads and how to protect your feet here.
Dry skin on the feet is typically caused by environmental or lifestyle factors, such as:
Unlike fungal infections, dry skin is not contagious and often responds well to over-the-counter moisturizers and hydration strategies.
Whether your feet are fighting fungus or just feeling dry, these habits will help protect and nourish them:
To help reduce your risk of fungal infections, follow these essential habits for nail and skin hygiene: 5 Ways to Keep Your Toenails Healthy and Fungus-Free.
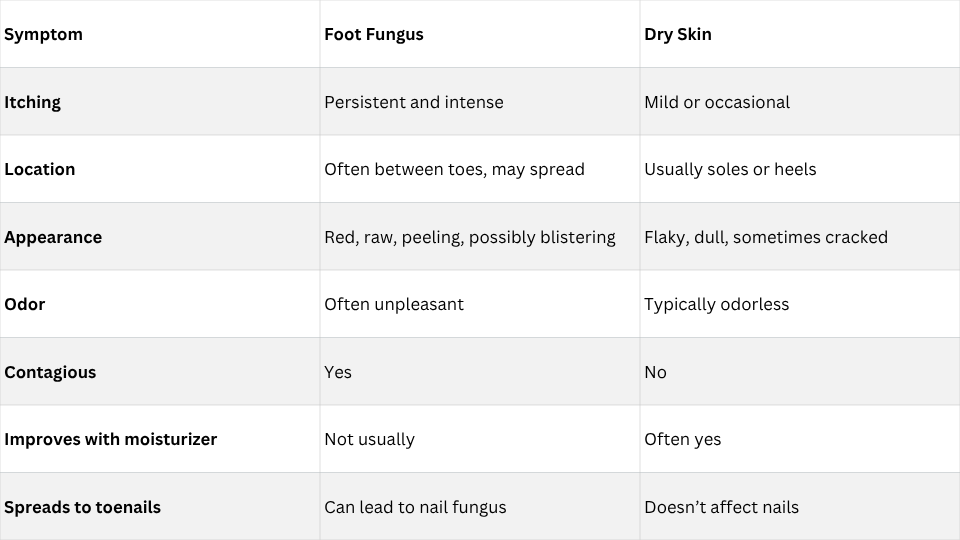
Here’s a side-by-side comparison to help you spot the difference:
If your symptoms are persistent or worsening, even with moisturizers, it could be more than just dry skin. For more prevention strategies, check out these tips on how to avoid the development of athlete’s foot and other foot fungus.

If you’re trying to decide whether your symptoms point to foot fungus vs dry skin, here are some practical ways to assess what’s going on:
Apply a rich, fragrance-free foot cream to the affected area twice a day for several days.
Fungal infections often hide between the toes. If the skin is:
While dry skin can itch mildly, persistent or intense itching (especially at night or after removing socks) leans more toward fungus.
Foot odor isn’t just a nuisance—it can be an important clue.
Fungal infections often produce a distinct unpleasant odor, while dry skin usually doesn’t smell at all.
Fungal infections can spread quickly to other areas of the foot, between toes, or even toenails.
Dry skin, on the other hand, tends to stay localized and improves with hydration.
You're more likely to have foot fungus if you:
If you're still unsure, it's best to see a podiatrist. A quick exam or skin test can confirm the diagnosis and get you started on the right treatment.
Some cases aren’t so cut-and-dry. You may be dealing with both dry skin and a fungal infection, or a more serious condition altogether.
Make an appointment with a podiatrist if:
At Foot & Ankle Specialists (FAS) The Woodlands, our podiatrists can help you determine what’s really going on with your skin and design a treatment plan tailored to your needs. Schedule a consultation today to get your foot skin and your comfort back on track.

Plantar fasciitis in pregnancy can cause heel pain and discomfort. Learn safe relief options, symptoms to watch for, and care guidance from FAS The Woodlands.